To read: ~ 5 minutes
Walk onto any surgical or critical care floor, and several constants stand out. There’s the synchronized rhythm of nurses and doctors working together, the quiet conversations at shift change, and the steady hum of monitors tracking every heartbeat. Yet in this methodical environment, one element stands in stark contrast — the piercing blare of alarms.
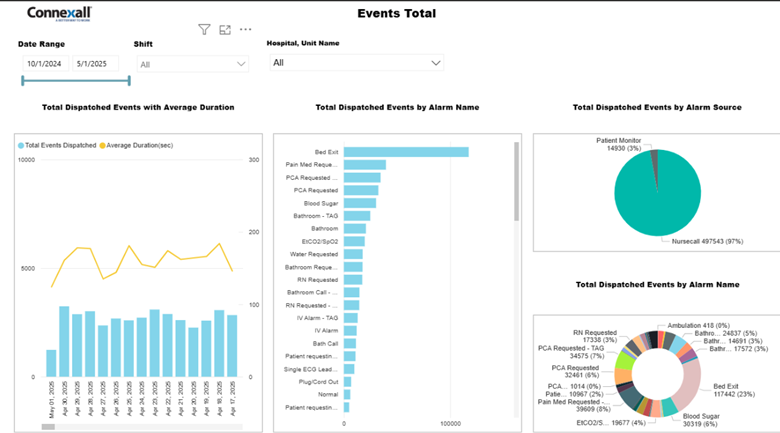
Alerts for everything from empty IV pumps to nurse calls to true patient emergencies echo across these departments, occurring (by some estimates) more than 350 times per patient per day.

Alarm fatigue is taking its toll. One recent study found that nurses who experience alarm fatigue have a 95% higher chance of burnout than those that don’t.
Alarm overload can create a dangerous cycle:
- Nursing staff bombarded with alarms become desensitized, and tune them out as background noise.
- Patient safety, quality of care, and functionality in clinical work environments are compromised by overwhelmed staff
- Administrators faced with staff shortages and tight budgets are unable or unwilling to roll out yet another software solution
- Operational complexity makes it extra difficult to establish consistent alarm management protocols across any given team
Leading hospitals recognize this cycle—and are looking for integrated solutions to tackle it.
Building a team of experts
Jan Capps (MSN, RN, PMP), Director of Clinical Services and Outcomes at Connexall, recognized that solving alarm fatigue required more than technical solutions. It needed an evidence-based approach to clinical workflow optimization.
In other words: hospitals needed solutions developed by former clinicians (like Jan) who deeply understood clients’ alarm fatigue and were committed to solving the problem.
That’s why Jan brought in a specialized team with diverse clinical backgrounds to build Clinical Elevate, Connexall’s solution to the alarm fatigue problem. She hired staff with ER, ICU, NICU, Cath lab, Interventional Radiology, Med-surg, and Surgical Services experience, as well as deep informatics training
“Everyone on my team are advanced practice nurses…most of us hold a master’s degree in nursing or nursing informatics. Everyone’s at least a BSN or higher.”
Once Jan’s high-performing brain trust was established, they set about developing four key elements as the foundation of their new clinical-first implementation:
- Evidence-based assessment tools — no flying in with new solutions unrelated to on-the-ground challenges
- Direct clinical observation, including more than 85 hours of client collaboration over the 12-month period
- Cross-functional stakeholder engagement to gain buy-in on both staff and leadership levels
- Sustainable workflow optimization that would create simpler, more effective processes to benefit staff in their day-to-day
How 12 months of deep listening transforms clinical workflows
A hospital is a living organism with a collection of systems that need to communicate and collaborate in order to keep everything running smoothly.
Hospitals looking to truly alleviate nurse burnout can take a page from Jan’s playbook when it comes to building processes that work for those different systems—and making them stick.
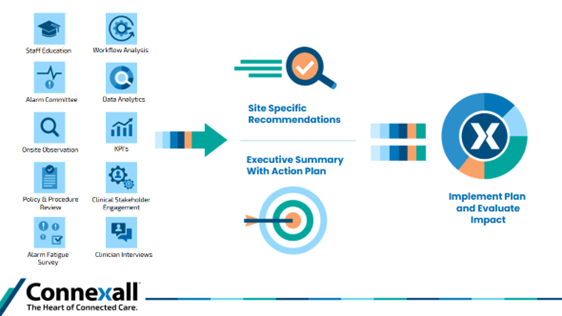
Asking questions to identify specific challenges (Phase 1, months 1–3)
Successful implementation begins by listening to understand specific challenges.
Jan’s team knows it’s the clinical staff who most intimately understand the problems with alarm management in their hospital. Nurses and team members know where the communication gaps are, where there’s not enough oversight, and where roles are unclear.
“In that first phase,” Jan says, “it’s all about stakeholder engagement, reviewing policies and procedures, reviewing how they educate and starting data analysis.”
During this phase, the Clinical Elevate team:
- Partners with clinical leadership to uncover acute pain points like alarm fatigue, alert distrust, and workflow workarounds.
- Assesses whether nurses are forced to self-triage excessive alerts or ignore non-critical notifications (is their first assumption “false alarm?”).
- Evaluates if siloed departments like telemetry monitoring and floor staff are effectively communicating, and whether a cycle of waiting for alarm confirmation (is this a “real real?”) is causing delays and impacting patient safety.
- Reviews whether current policies empower or restrict staff from adjusting alert parameters based on clinical judgment, and if alarm response protocol roles are clear.
Once the analysis is complete, Connexall’s Clinical Elevate team of specialist’s help establish (or revitalize) a dedicated alarm committee with regular meetings and a new mandate: reducing fatigue and refining SOPs.
But, the goal isn’t to barge in and overhaul. Great clinical environments thrive on a balance of protocols and real-time decision-making. That’s why Connexall’s Clinical Elevate team leads with a human-centric mindset—one that prioritizes the needs of both patients and caregivers. Guided by principles of partnership, active listening, and human factors engineering, we work alongside clients to understand what truly works for the people delivering and receiving care.
Spend time making direct observations (Phase 2, months 4–6)
In the second phase of implementation, experienced clinical solution specialists observe on-site workflows and evaluate any physical/environmental factors that might impact communication.
This means going beyond surface-level assessments to understand the real-world workflow—the difference between work imagined and work done. Connexall’s Clinical Elevate team focuses on identifying system inefficiencies by closely observing how clinicians engage with their tools, technology, and environment to complete tasks. This includes:
- Communication breakdowns during handoff transitions
- Friction points in cross-departmental interactions
- The physical layout of the unit and its impact on clinician movement and tech use
- Staffing patterns and how they shape technology adoption at the bedside
This phase is all about close partnership: “It’s our clinical solution specialists—seasoned in informatics—working shoulder to shoulder with bedside clinicians to bridge the gap between technology and real-world care,” says Jan.
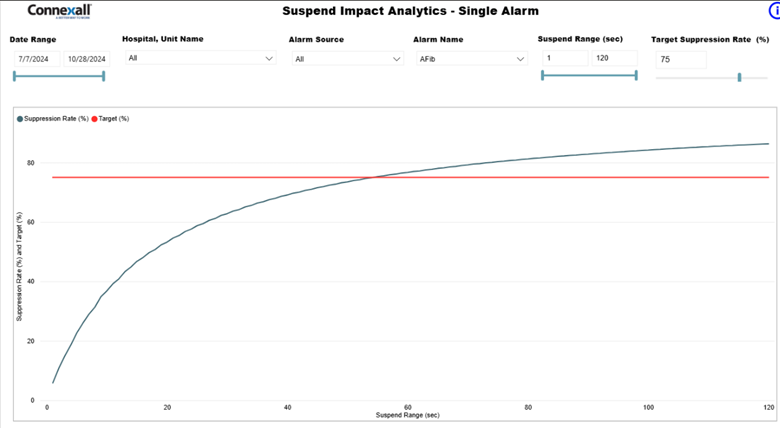
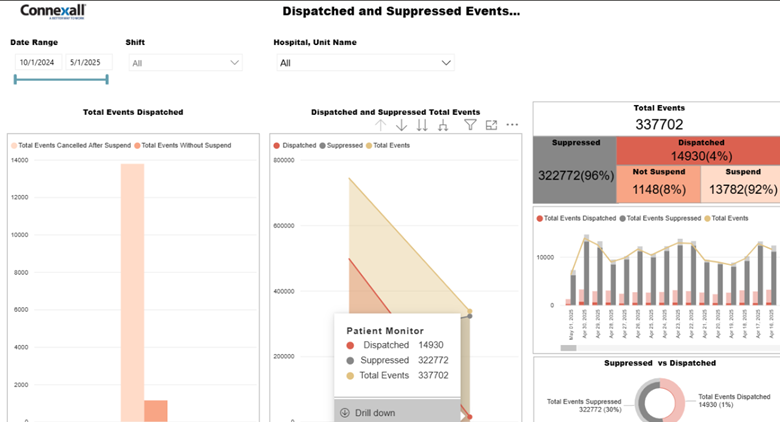
Deep data analysis (Phase 3, months 7–12)
Your data analysis is only as good as your underlying data.
Fortunately, when you spend enough upfront time in the information-gathering and direct observation phases, your data can get pretty darn good.
In the final phase, Connexall’s Clinical team ingests and analyzes all insights to deliver measurable improvements. Data specialists on the team dig into data and analytics, look at configurations, and make recommendations for system updates and changes.
Critical components include:
- Targeted workflow changes alongside continuous monitoring
- Team-led education and change management support
- A collaborative 90-day stabilization period with follow-up assessments
For Jan, the stabilization period is particularly important. “It’s where you ensure adoption,” she explains. “That’s where you unearth if something could have or should have been done differently.”
The sound of silence: 43% reduction in alarm fatigue for Novant
This clinical-first implementation approach delivered powerful results at Novant Health. Since the initial rollout, Novant has expanded the Clinical Elevate program to twelve facilities, achieving a 43% reduction in alarms across sites.
The change for Novant was so dramatic, it took their staff a moment to remember the sound of silence..
Nurses–used to the constant blare of unnecessary alarms—went into vacant rooms to turn on monitors and set off alarms themselves to make sure nothing was broken. Turned out nothing was, except the old way of doing things.
Success Through Human-Centered Implementation
The key to these results wasn’t just technology, it was applying human factors engineering principles through contextual inquiries. By observing clinicians in their real environments, understanding the “why” behind their workflows, and identifying hidden inefficiencies, we were able to analyze and improve the system in ways that truly support the people who use it.
“The technology we deploy is one very, very small piece.” Jan says. Operational readiness, clinical adoption, and training come first, and make the biggest impact.
Their biggest learnings from a clinical-first approach:
Trust and vulnerability matter. Invest in the humans behind the product: the staff and patients most directly impacted by the technology. Their on-the-ground input will drive more change than any algorithm.
Stakeholder engagement = adoption. Involve stakeholders even when decisions are predetermined. “We all want to be involved in decisions that impact our day to day work.” Jan says. This is about human beings making behavioral changes. People want to feel listened to—even if they’re not the final decision-maker.
Clinical expertise builds credibility. The 12-month Clinical Elevate engagement is purposefully designed to both win-over reluctant users, and empower clients to eventually become fully self-sufficient in their alarm management protocols.
Technical changes alone won’t solve alarm fatigue, and leading hospitals recognize that cultural and educational changes are just as important.
With Clinical Elevate they’ve created a technology and an onboarding process that serves people, rather than forcing yet another set of complex systems on already stretched hospital staff.
Their success is evident, with nine engagements already underway this year.
And the sound of that success? For once: silence.